The World Health Organization’s recent classification of hepatitis D virus (HDV) as carcinogenic to humans marks a pivotal moment in global health policy and liver cancer prevention. This groundbreaking announcement, made on World Hepatitis Day 2025, elevates hepatitis D to the same classification level as hepatitis B and C viruses, underscoring its significant role in liver cancer development.The classification by the International Agency for Research on Cancer (IARC) as Group 1 carcinogenic is based on compelling evidence showing that HDV infection increases liver cancer risk by two- to six-fold compared to hepatitis B virus (HBV) infection alone. This development has profound implications for the estimated 48-60 million people worldwide living with HDV infection, particularly those in low- and middle-income countries where the burden is highest.
Understanding Hepatitis D Virus and Its Carcinogenic Nature
The Unique Biology of HDV
Hepatitis D virus represents one of the most unusual pathogens affecting humans, being classified as a defective RNA virus that cannot complete its life cycle independently. HDV possesses a circular, single-stranded RNA genome of approximately 1,679 nucleotides, making it the smallest known human pathogen. The virus encodes only one protein, the hepatitis delta antigen (HDAg), which exists in two forms: small HDAg (S-HDAg) and large HDAg (L-HDAg). This obligate dependence on HBV for replication and transmission creates a unique epidemiological pattern where HDV infection can only occur in individuals already infected with hepatitis B.
The dependency relationship between HDV and HBV is complex and bidirectional. While HDV requires HBV surface antigens for virion assembly and hepatocyte entry, HDV infection often suppresses HBV replication through competitive mechanisms. However, this suppression is not sustained throughout the disease course, and studies show that significant HBV replication can be detected in approximately half of HDV-infected patients over time8. This interplay between the two viruses contributes to the severe clinical outcomes observed in coinfected patients.
Mechanisms of HDV-Induced Carcinogenesis
Recent molecular studies have revealed that HDV promotes liver cancer through distinct pathways compared to other hepatitis viruses. Unlike HBV, which can integrate into the host genome and directly activate oncogenic pathways, HDV appears to drive carcinogenesis primarily through genetic instability mechanisms. Transcriptomic analysis of HDV-associated hepatocellular carcinoma (HCC) has identified a unique molecular signature characterized by upregulation of genes involved in cell cycle regulation, DNA replication, damage, and repair.
The large hepatitis delta antigen (L-HDAg) plays a crucial role in oncogenic processes by activating multiple cellular signaling pathways. L-HDAg stimulates the STAT3 and NF-κB pathways, which are known to promote cell survival, proliferation, and transformation. Additionally, L-HDAg induces oxidative stress through activation of NADPH oxidase-4 (NOX-4), leading to reactive oxygen species production that can damage DNA and promote malignant transformation.
Epigenetic modifications represent another important mechanism of HDV-induced carcinogenesis. Both small and large HDV antigens enhance histone H3 acetylation in the clusterin gene promoter, leading to increased clusterin expression. Clusterin is a cytoprotective protein that is commonly upregulated in various cancers and promotes cell survival under stress conditions8. Furthermore, L-HDAg activates DNA methyltransferases (DNMT1 and DNMT3b), which can silence tumor suppressor genes through hypermethylation.
Epidemiological Evidence for HDV Carcinogenicity
Global Burden and Cancer Risk
The evidence supporting HDV’s carcinogenic classification comes from multiple epidemiological studies demonstrating consistently elevated cancer risks in HDV-infected patients. A comprehensive meta-analysis involving over 63,000 patients found that individuals with HBV/HDV coinfection had a two-fold increased risk of developing hepatocellular carcinoma compared to those with HBV monoinfection alone. More specifically, several large-scale studies have reported relative risks ranging from 2.9 to 6.1 for HCC development in HDV-coinfected patients.
The Swedish population-based study, one of the largest cohorts to date, included 9,160 HBV patients and 650 with HDV infection, demonstrating significantly higher HCC risk in both acute and chronic HDV infection after adjusting for age. Similarly, a study of American veterans found a 2.9-fold higher incidence of HCC in HDV-positive individuals even after adjusting for cirrhosis and hepatitis C coinfection. These findings are particularly significant because they account for other known liver cancer risk factors, suggesting that HDV contributes independently to carcinogenesis.
Accelerated Disease Progression
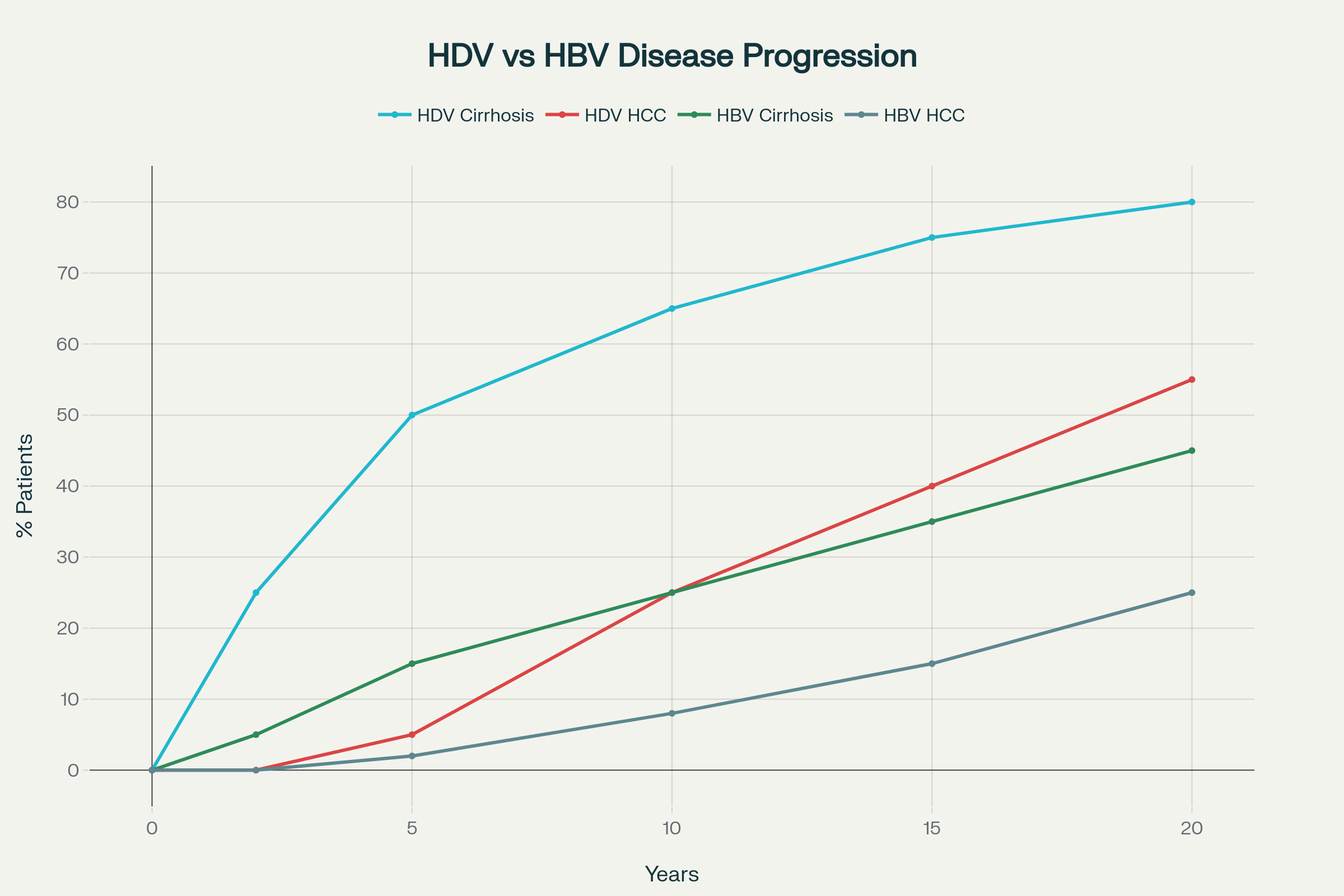
HDV infection is characterized by rapid progression to severe liver disease, with studies showing that 75% of HDV patients develop cirrhosis within 15 years compared to slower progression in HBV monoinfection. The progression to hepatocellular carcinoma typically occurs within 10 years of infection, significantly faster than other forms of viral hepatitis. This accelerated timeline has important implications for screening and surveillance strategies, as patients may develop advanced liver disease and cancer at younger ages than those with other chronic liver conditions.
The risk of liver decompensation and death is also substantially higher in HDV-infected patients. Studies have shown that HDV coinfection increases the risk of cirrhosis by 3-10 times compared to HBV monoinfection. Furthermore, the annual rates of progression to cirrhosis and HCC in HDV patients are approximately 4% and 2.8% respectively, indicating a relentless disease progression that underscores the urgent need for effective interventions.
Molecular Pathways and Oncogenic Mechanisms
Genetic Instability as a Driver
Advanced molecular analysis has revealed that HDV-associated HCC exhibits a distinct genetic profile characterized by widespread chromosomal instability and DNA damage. The upregulation of multiple DNA repair pathways, including GADD45, cell cycle checkpoint controls, and hereditary breast cancer pathways, suggests that HDV infection creates a cellular environment prone to genetic mutations and malignant transformation. This finding is particularly significant because it differentiates HDV-induced carcinogenesis from that caused by HBV or HCV, despite HDV’s obligate dependence on HBV.
The activation of the Sonic Hedgehog pathway in HDV-associated tumors represents another unique feature of this form of liver cancer. This developmental signaling pathway is rarely activated in other types of HCC, suggesting that HDV may hijack specific cellular programs to promote tumorigenesis. The strong coregulation of genes involved in DNA replication and repair indicates that HDV creates a coordinated cellular response that paradoxically promotes genomic instability while attempting to maintain cell viability.
Inflammatory and Fibrotic Pathways
HDV infection induces severe necroinflammation that exceeds that seen in other forms of viral hepatitis. The chronic inflammatory state is mediated through multiple pathways, including TNF-α-induced NF-κB activation and complement system dysregulation. This persistent inflammation creates a microenvironment rich in cytokines, chemokines, and reactive oxygen species that promote hepatocyte damage, compensatory proliferation, and eventually malignant transformation.
The fibrotic response in HDV infection is particularly aggressive, with rapid progression from inflammation to cirrhosis. L-HDAg activates transforming growth factor-β (TGF-β) signaling pathways through interaction with Smad3, promoting epithelial-to-mesenchymal transition and excessive collagen deposition. The combination of chronic inflammation and progressive fibrosis creates a perfect storm for cancer development, as the liver attempts to regenerate in an environment of ongoing tissue damage and architectural distortion.
Global Health Impact and Regional Distribution
Geographic Patterns of HDV Burden
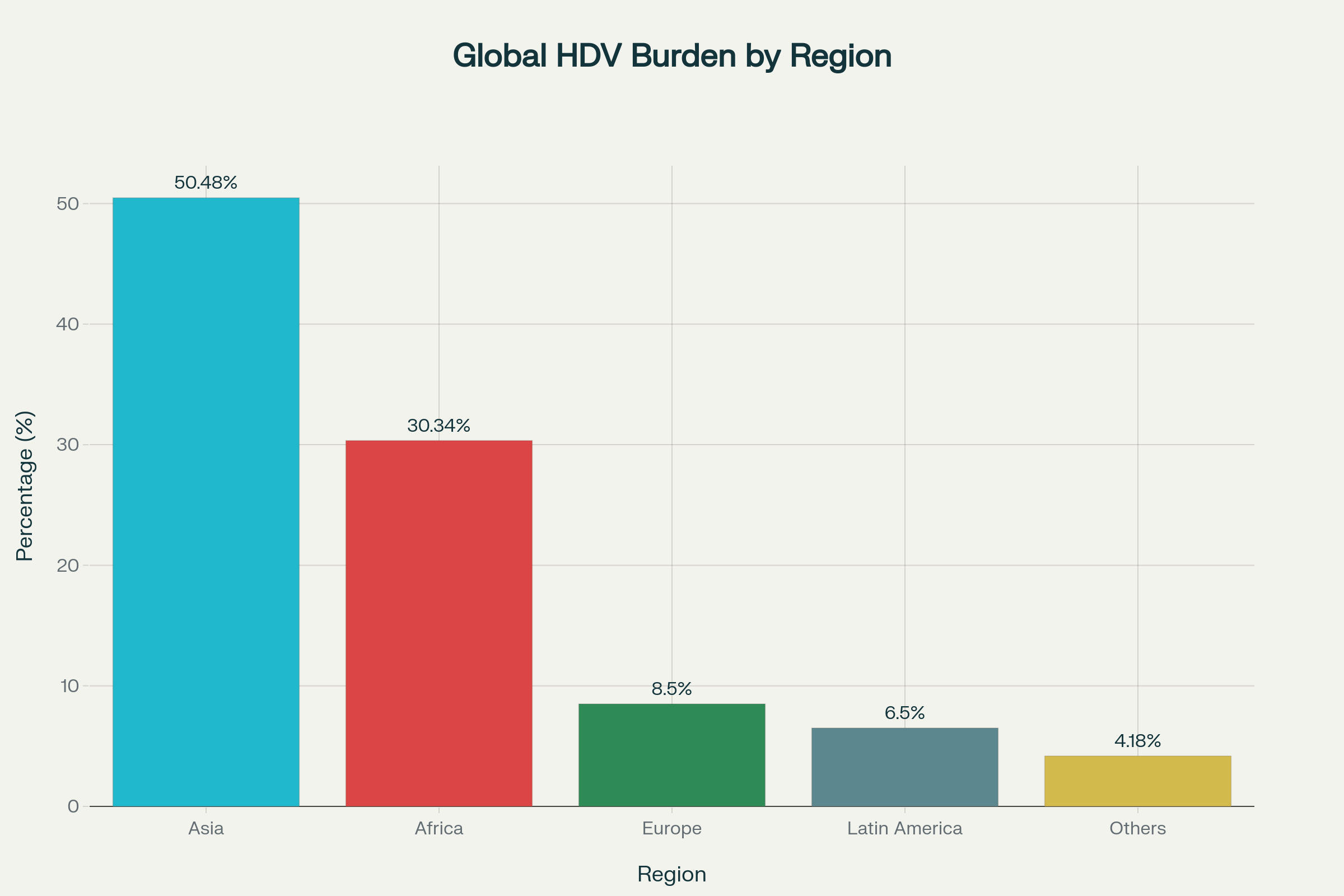
The global distribution of HDV infection shows marked geographical variation, with Asia accounting for 44-57% of all cases and Africa contributing 22-38% of the global burden4. This uneven distribution reflects historical patterns of HBV transmission, migration patterns, and varying effectiveness of hepatitis B vaccination programs. High-prevalence regions include Central Asia, Eastern Europe, the Mediterranean basin, parts of South America, and sub-Saharan Africa.
Recent epidemiological trends suggest that HDV prevalence may be increasing in traditionally low-prevalence areas due to global migration patterns. Studies from European countries have documented rising HDV prevalence among immigrant populations, highlighting the need for universal screening approaches rather than risk-based testing strategies. This changing epidemiology has important implications for healthcare systems that may not be prepared to diagnose and manage HDV infection in their patient populations.
Population-Specific Risks
Certain populations face disproportionately high risks of HDV infection and subsequent liver cancer development. People who inject drugs (PWID) show HDV prevalence rates of 37.57% among HBV-positive individuals, representing a 15-fold increased risk compared to the general HBV-infected population. Men who have sex with men, individuals with multiple sexual partners, and those with HIV coinfection also demonstrate elevated HDV prevalence rates.
The interaction between HIV and HDV creates particularly concerning outcomes, with triple-infected patients (HIV/HBV/HDV) showing a six-fold increased risk of HCC compared to HIV/HBV coinfected individuals. This finding highlights the importance of comprehensive hepatitis screening in HIV-positive populations and the need for integrated care models that address multiple viral infections simultaneously.
Diagnostic Approaches and Screening Strategies
Current Testing Methodologies
HDV diagnosis relies primarily on serological testing for anti-HDV antibodies followed by molecular detection of HDV RNA in positive cases. The initial screening uses enzyme-linked immunosorbent assays (ELISA) to detect total anti-HDV antibodies, which persist long after infection and can indicate either current or past HDV exposure. Confirmation requires quantitative HDV RNA testing using reverse transcription polymerase chain reaction (RT-PCR) methods.
The World Health Organization established the first international standard for HDV RNA quantification in 2013, which has improved the standardization and comparability of HDV testing globally2126. However, significant challenges remain in test availability and standardization, particularly in resource-limited settings where HDV burden is highest. Many laboratories still rely on in-house assays that lack adequate validation and standardization, leading to inconsistent results and potential underdiagnosis.
Screening Guidelines and Recommendations
Current screening recommendations vary significantly between professional organizations and geographic regions. The American Association for the Study of Liver Diseases (AASLD) recommends risk-based screening for HDV in HBV-positive patients, focusing on high-risk groups such as people who inject drugs and immigrants from endemic areas. In contrast, the European Association for the Study of the Liver (EASL) and several expert panels now recommend universal screening of all HBsAg-positive individuals.
The Chronic Liver Disease Foundation has issued the strongest recommendation for universal HDV screening, arguing that risk-based approaches miss significant numbers of infected individuals and that universal testing is more practical for healthcare providers who may not be familiar with HDV epidemiology. This approach is supported by evidence showing that HDV infection occurs in patients without traditional risk factors and that the consequences of missed diagnosis are severe.
Treatment Advances and Cancer Prevention
Established Therapeutic Options
Pegylated interferon-alpha (PEG-IFN-α) has been the standard treatment for chronic HDV infection for many years, despite limited efficacy and significant side effects. Treatment duration typically ranges from 12-48 months, with sustained virological response rates of 25-40% at 24 weeks post-treatment. While some patients achieve HDV RNA clearance, relapse rates exceed 50% in many studies, highlighting the need for more effective therapeutic approaches.
The primary treatment goal is achieving at least a 2-log reduction in HDV RNA levels, which correlates with improved clinical outcomes including reduced liver inflammation and slower disease progression. Patients who achieve this virological milestone show decreased risk of cirrhosis development and potentially reduced HCC risk, although long-term cancer prevention data are still limited.
Bulevirtide: A Breakthrough in HDV Treatment
Bulevirtide (Hepcludex) represents a paradigm shift in HDV treatment as the first specifically approved therapy for chronic hepatitis D. This first-in-class entry inhibitor works by binding to and inactivating the sodium-taurocholate co-transporting polypeptide (NTCP) receptor, preventing HDV and HBV entry into hepatocytes. The drug received conditional approval in the European Union in 2020 based on demonstrated efficacy and safety in phase III trials.
Clinical trial data show that bulevirtide achieves virological response rates of 71-76% at 48 weeks, significantly higher than historical controls with PEG-IFN-α. The 2 mg and 10 mg daily dosing regimens both demonstrate substantial HDV RNA reductions, with some patients achieving undetectable viral loads. Long-term treatment appears to be well-tolerated, with the main side effect being reversible elevation of bile acids due to NTCP inhibition.
Cancer Prevention Potential
While definitive data on cancer prevention are still emerging, early evidence suggests that effective HDV treatment may reduce HCC risk. A retrospective economic analysis projected that bulevirtide treatment could prevent 113 HCC cases per 3,882 treated patients over a lifetime compared to PEG-IFN-α. Long-term studies are ongoing to establish whether sustained HDV suppression translates into meaningful reductions in liver cancer incidence.
The stabilization of liver function observed in bulevirtide-treated patients provides encouraging evidence for cancer prevention potential. Studies show that Child-Pugh and MELD scores remain stable or improve in most patients receiving long-term bulevirtide therapy, with only rare cases of hepatic decompensation during treatment. This functional improvement suggests that effective antiviral therapy may interrupt the progression pathway from chronic inflammation to cirrhosis and cancer.
Prevention Strategies and Public Health Implications
Hepatitis B Vaccination as Primary Prevention
Since HDV cannot infect individuals without concurrent HBV infection, hepatitis B vaccination represents the most effective primary prevention strategy for HDV. Universal childhood HBV vaccination programs have successfully reduced HDV incidence in many regions, as evidenced by the age-related shift in HDV prevalence toward older individuals in vaccinated populations. Countries with high vaccination coverage rates have documented substantial reductions in both HBV and HDV transmission.
However, significant gaps remain in global HBV vaccination coverage, particularly among adults and high-risk populations. The COVID-19 pandemic has further disrupted vaccination programs, potentially expanding the pool of individuals susceptible to HDV infection. Addressing these gaps requires sustained commitment to vaccination programs, catch-up immunization for unvaccinated adults, and targeted interventions for high-risk populations such as people who inject drugs.
Secondary Prevention Through Screening
Early detection through systematic screening represents the second line of defense against HDV-related liver cancer. Universal screening of HBsAg-positive individuals could identify infected patients before significant liver damage occurs, enabling early intervention and potentially preventing cancer development. The implementation of reflexive HDV RNA testing for all anti-HDV positive results could streamline the diagnostic process and improve linkage to care.
Healthcare provider education remains a critical component of effective screening programs, as awareness of HDV among clinicians is generally low. Studies show that HDV testing is most likely to be ordered by gastroenterologists and infectious disease specialists, but high-risk patients often receive care from other specialties that may not routinely consider HDV testing. Comprehensive educational initiatives targeting primary care providers, emergency medicine physicians, and addiction specialists could significantly improve screening rates.
Hepatocellular Carcinoma Surveillance
For patients already infected with HDV, regular surveillance for hepatocellular carcinoma represents an essential tertiary prevention strategy. Current guidelines recommend ultrasound screening every 6 months for HDV patients with advanced fibrosis or cirrhosis, similar to recommendations for other chronic liver diseases. However, the accelerated progression of HDV-related liver disease may warrant more intensive surveillance protocols or earlier initiation of screening.
The optimal age to begin HCC surveillance in HDV patients remains unclear, as these individuals often develop cancer at younger ages than those with other liver diseases. Some experts suggest that surveillance should begin earlier in HDV patients, particularly those with additional risk factors such as alcohol use, obesity, or viral coinfections. The development of improved biomarkers and imaging techniques may enable more precise risk stratification and personalized surveillance strategies in the future.
Future Directions and Research Priorities
Advancing Treatment Options
While bulevirtide represents a significant advance, several limitations remain that drive continued research efforts. Current treatment requires indefinite duration, as viral rebound typically occurs after discontinuation. Combination therapies pairing bulevirtide with other antiviral agents or immunomodulators may achieve more durable responses and potentially enable finite treatment regimens.
Novel therapeutic targets under investigation include RNA interference approaches, capsid assembly inhibitors, and immune-based therapies. The unique biology of HDV, particularly its dependence on host RNA polymerase II for replication, offers potential targets that could be exploited without affecting normal cellular functions. Additionally, therapeutic strategies aimed at achieving HBV cure could simultaneously eliminate HDV, representing the ultimate treatment goal.
Improving Diagnostic Capabilities
The development of point-of-care testing for HDV could revolutionize screening programs, particularly in resource-limited settings where laboratory infrastructure is limited. Rapid diagnostic tests similar to those available for HIV and hepatitis C could enable immediate diagnosis and treatment initiation in clinical settings. Additionally, improved assays capable of detecting all HDV genotypes with equal sensitivity are needed to ensure accurate diagnosis across different geographic regions.
Understanding Long-term Outcomes
Longitudinal studies following HDV patients for decades are needed to fully understand the natural history of infection and the impact of effective treatment on cancer prevention. These studies should include detailed molecular characterization of tumors that develop despite treatment, genetic factors that influence disease progression, and optimal surveillance strategies for different patient populations. Additionally, real-world effectiveness studies of bulevirtide and other emerging therapies are essential to guide clinical practice and health policy decisions.
Conclusion
The WHO’s classification of hepatitis D virus as carcinogenic represents a watershed moment in recognizing the significant cancer risk posed by this often-overlooked pathogen. With compelling evidence showing a 2-6 fold increased risk of liver cancer compared to hepatitis B infection alone, HDV now joins hepatitis B and C in the highest category of human carcinogens. This classification is supported by robust epidemiological data from multiple large-scale studies and emerging molecular evidence demonstrating distinct pathways of HDV-induced carcinogenesis.
The global burden of HDV infection, affecting an estimated 48-60 million people worldwide, concentrated primarily in Asia and Africa, demands urgent public health action. The rapid progression from infection to cirrhosis (within 5 years) and hepatocellular carcinoma (within 10 years) underscores the aggressive nature of this disease and the critical importance of early detection and intervention. Recent therapeutic advances, particularly the approval of bulevirtide as the first specific HDV treatment, offer new hope for cancer prevention through effective viral suppression.
Moving forward, comprehensive strategies encompassing universal hepatitis B vaccination, systematic HDV screening of all HBsAg-positive individuals, early treatment with effective antivirals, and regular cancer surveillance represent our best tools for combating this newly recognized carcinogen202422. The integration of HDV into global hepatitis elimination strategies and cancer prevention programs will be essential to reduce the burden of liver cancer and save lives in the millions of people affected by this serious infection worldwide.
Updated on August 13, 2025 with latest context.